Fosfomycin in UTI Management: A Modern Approach to an Age-Old Problem
Urinary tract infections (UTIs) remain one of the most prevalent infectious diseases worldwide, affecting millions annually. They account for a significant portion of outpatient prescriptions and pose a growing public health challenge due to the alarming rise of antimicrobial resistance (AMR).
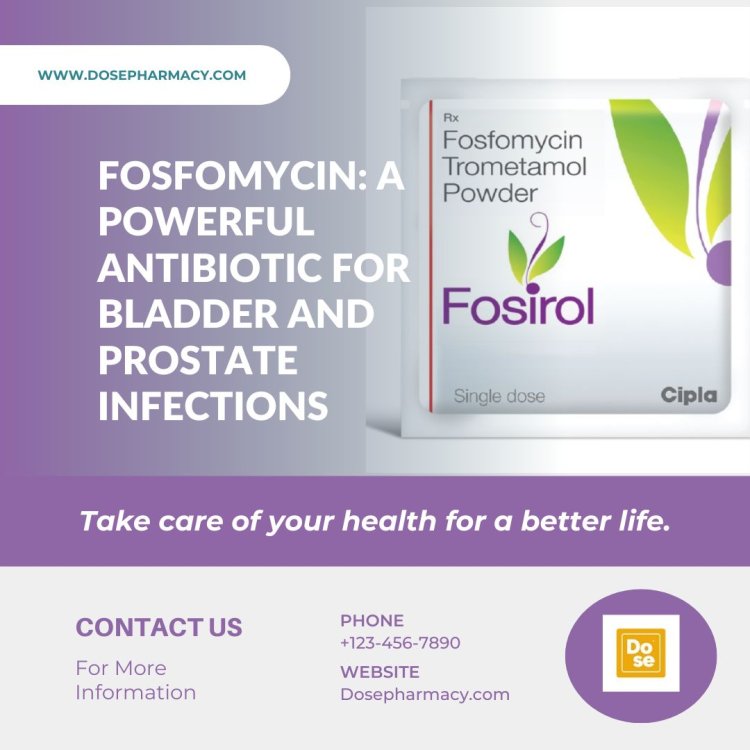
Urinary tract infections (UTIs) remain one of the most prevalent infectious diseases worldwide, affecting millions annually. They account for a significant portion of outpatient prescriptions and pose a growing public health challenge due to the alarming rise of antimicrobial resistance (AMR). Among the arsenal of antibiotics, fosfomycin has gained renewed interest as an effective and well-tolerated treatment option for UTIs, particularly in the era of multidrug-resistant (MDR) pathogens. This article explores the historical development, mechanism of action, clinical applications, and potential limitations of fosfomycin in managing UTIs, offering a modern perspective on this old antibiotic.
Historical Background and Development
Fosfomycin was first discovered in 1969 from cultures of Streptomyces fradiae. Its unique chemical structure—an epoxide moiety—set it apart from other antibiotics. Initially overshadowed by newer antibiotics, fosfomycin saw limited use in clinical practice. However, as resistance to traditional first-line antibiotics like fluoroquinolones and beta-lactams surged, fosfomycin re-emerged as a vital therapeutic agent for challenging infections.
Approved for use in over 40 countries, fosfomycin has been primarily used in its oral formulation (fosfomycin tromethamine) for uncomplicated UTIs and its intravenous form (fosfomycin disodium) for more severe infections. Its resurgence reflects a broader trend of revisiting older antibiotics to address the AMR crisis.
Mechanism of Action and Spectrum of Activity
Fosfomycin’s bactericidal action stems from inhibiting the bacterial enzyme UDP-N-acetylglucosamine enolpyruvyl transferase (MurA). This enzyme plays a crucial role in the initial steps of peptidoglycan synthesis, which is essential for bacterial cell wall integrity. Fosfomycin disrupts cell wall synthesis by irreversibly binding to MurA, leading to bacterial lysis.
Broad Spectrum of Activity
Fosfomycin 3gm sachet exhibits activity against a wide range of Gram-positive and Gram-negative pathogens, including:
-
Enterobacterales (e.g., Escherichia coli, Klebsiella pneumoniae)
-
Multidrug-resistant strains, such as extended-spectrum beta-lactamase (ESBL)-producing E. coli and Klebsiella spp.
-
Carbapenem-resistant Enterobacterales (CRE)
-
Certain Gram-positive organisms, such as methicillin-resistant Staphylococcus aureus (MRSA)
This broad spectrum and its ability to retain efficacy against MDR pathogens make fosfomycin particularly valuable in the current antimicrobial landscape.
Clinical Applications in UTI Management
Uncomplicated UTIs
Fosfomycin tromethamine is a first-line treatment for uncomplicated UTIs, particularly in women. A single 3-gram oral dose has proven highly effective, achieving cure rates comparable to other first-line agents like nitrofurantoin. Advantages include:
-
Convenience: A single-dose regimen improves patient adherence.
-
Safety: Fosfomycin is well-tolerated, with minimal side effects.
-
Efficacy: Effective against both typical UTI pathogens and ESBL-producing strains.
Complicated UTIs and Pyelonephritis
While fosfomycin’s oral form is less frequently used for complicated UTIs or pyelonephritis, its intravenous formulation offers a promising alternative. Intravenous fosfomycin has demonstrated success in combination therapies for treating:
-
Severe, complicated UTIs
-
Urosepsis
-
Infections caused by CRE or other MDR organisms
Recurrent UTIs
Fosfomycin also plays a role in managing recurrent UTIs, especially when traditional prophylactic agents fail or resistance limits options. Its unique mechanism of action and low propensity for resistance development make it an attractive choice for intermittent or long-term prophylaxis.
Pharmacokinetics and Pharmacodynamics
Fosfomycin exhibits favorable pharmacokinetic and pharmacodynamic properties for UTI management:
-
High Urinary Concentrations: After oral administration, fosfomycin achieves peak urinary concentrations within 4 hours, maintaining therapeutic levels for up to 48 hours.
-
Wide Distribution: The drug penetrates well into tissues, including the kidneys and bladder wall.
-
Low Protein Binding: Minimal protein binding enhances its bactericidal activity.
These properties ensure fosfomycin’s efficacy in eradicating uropathogens in both uncomplicated and complicated UTIs.
Resistance Mechanisms and Concerns
Despite its advantages, resistance to fosfomycin is not uncommon, particularly among hospital-acquired pathogens. Mechanisms of resistance include:
-
Target Modification: Mutations in the murA gene reduce fosfomycin’s binding affinity.
-
Enzymatic Inactivation: Fosfomycin-modifying enzymes, such as FosA, deactivate the antibiotic.
-
Reduced Permeability: Mutations in bacterial transporters (e.g., GlpT and UhpT) hinder fosfomycin’s uptake.
Addressing Resistance
To mitigate resistance, fosfomycin is often used as part of combination therapy, particularly for severe infections. Ongoing surveillance and judicious use are crucial to preserving its efficacy.
Safety and Tolerability
Fosfomycin is generally well-tolerated, with a low incidence of adverse effects. Common side effects include mild gastrointestinal disturbances (e.g., diarrhea, nausea) and headache. Rare but serious reactions, such as hypersensitivity, have been reported but remain uncommon.
Its safety profile makes fosfomycin suitable for use in various populations, including:
-
Pregnant women (FDA Category B)
-
Elderly patients
-
Individuals with renal impairment (dose adjustments may be necessary)
Advantages and Limitations
Advantages
-
Broad Spectrum: Effective against MDR pathogens.
-
Convenient Dosing: Single-dose regimen for uncomplicated UTIs.
-
Safety: Minimal side effects and high tolerability.
-
Unique Mechanism: Low cross-resistance with other antibiotics.
Limitations
-
Resistance Development: Rising resistance in certain settings.
-
Limited Availability: Intravenous formulation is not widely available in some regions.
-
Narrow Indications: Oral form is primarily limited to uncomplicated UTIs.
Future Directions and Research
The growing interest in fosfomycin has spurred research into its expanded use and optimization. Key areas of focus include:
-
Combination Therapies: Investigating synergistic effects with other antibiotics to combat MDR infections.
-
Extended Indications: Exploring its role in treating non-UTI infections, such as respiratory and bone infections.
-
Resistance Surveillance: Monitoring global resistance trends to guide clinical use.
-
Formulation Improvements: Developing novel delivery systems to enhance efficacy and bioavailability.
Conclusion
Fosfomycin represents a modern solution to an enduring problem in infectious disease management. Its unique properties, broad-spectrum activity, and safety profile make it an indispensable tool in the fight against UTIs, especially those caused by MDR pathogens. However, careful stewardship is essential to maximize its utility and prevent resistance. As research continues to unlock its full potential, fosfomycin stands poised to remain a cornerstone of UTI management in the era of AMR. Read More....
What's Your Reaction?













.jpg)